Modern Ayurveda Insights
Explore a data-driven approach to Ayurveda for a healthier, balanced lifestyle.


Trusted by 5,000+ users
★★★★★
A NEW AGE OF AYURVEDA
A Data-Driven Approach to the Modernization of Ayurveda
A NEW AGE OF WELLNESS
A Data-Driven Approach to the Modernization of Ayurveda
A NEW AGE OF WELLNESS
A Data-Driven Approach to the Modernization of Ayurveda

ABOUT SANTHIGRAM WELLNESS
Santhigram Kerala Ayurveda – is the world’s premier Ayurveda Wellness provider for a healthy body and mind, promoting the goodness of Ayurveda worldwide and providing the best treatments and services available in our day and time. Rapidly expanding from 12 locations in the United States and India, it has been recognized by the State of New Jersey as “an essential and superb holistic health organization” and is a member of NAMASTA (North American Studio Alliance), NAMA (National Ayurvedic Medical Association), AAPNA (Association of Ayurvedic Professionals of North America), and the AMTA (American Massage Therapy Association).
150+
15
Trusted by Experts
Join Us
What is Ayurveda?
India has a rich heritage spanning over 5,000 years in traditional medicinal systems like Ayurveda. It is a holistic and complete system for maintaining, balancing, and restoring health. The 8 dimensions of wellness advocated by Ayurveda include physical, mental, environmental, social, emotional, vocational, financial, and spiritual. Ayurvedic practices aim to promote a state of complete well-being combined with lifestyle choices that are characterized by personal responsibility and the optimal enhancement of physical, mental, and spiritual health.
Ayurveda utilizes natural healing methods that are tailored to the individual and advocates preventive measures through customized diet, lifestyle, and medicines. The applications of Ayurveda include constitution analysis (physiological and psychological), disease diagnostics and treatment, and diet and lifestyle advice. Ayurveda has been built around the concepts of personalized medicine based upon genomics and a systems view of human health.


The following ‘Systems Ayurveda’ graphic notation is a schema of the Ayurveda knowledge base. ‘Systems Ayurveda’ is an entity relationship notation based on Systems Biology Graphical Notation (SBGN). The holistic approach of Ayurveda management aims at establishing health through multifarious treatment modalities including counselling, avoiding causes, Panchakarma, medicines, diet and surgical procedures. Every aspect of ‘Systems Ayurveda’ logic is linked to other components and has a specific role in maintenance of health or treating diseases.
Tap image to enlarge
SANTHIGRAM FOUNDATION
The Santhigram Foundation – is a 501c3 charitable foundation for advocating and promoting health and wellness and raising awareness of the benefits of complementary and alternative medicine based on Ayurveda through research, data science, and dissemination of scientific information. The Santhigram Foundation provides nonmonetary support to medical research organizations and makes treatments more accessible to those suffering from chronic ailments..
Santhigram Kerala Ayurveda – is the world’s premier Ayurveda Wellness provider for a healthy body and mind, promoting the goodness of Ayurveda worldwide and providing the best treatments and services available in our day and time. Rapidly expanding from 12 locations in the United States and India, it has been recognized by the State of New Jersey as “an essential and superb holistic health organization” and is a member of NAMASTA (North American Studio Alliance), NAMA (National Ayurvedic Medical Association), AAPNA (Association of Ayurvedic Professionals of North America), and the AMTA (American Massage Therapy Association).
Santhigram Kerala Ayurveda
Santhigram Wellness Online – is a Delaware C Corp providing a HIPAA-compliant smart contracts platform for patient records and management with a Software-as-a-Service (SaaS) wellness app for patient diagnostics, health, and monitoring which also provides for data collection and data discovery with tokenized incentives to the user community. It is the digital development arm of the research performed by the Santhigram Foundation.
Santhigram Wellness Online





The Santhigram Foundation – is a 501c3 charitable foundation for advocating and promoting health and wellness and raising awareness of the benefits of complementary and alternative medicine based on Ayurveda through research, data science, and dissemination of scientific information. The Santhigram Foundation provides nonmonetary support to medical research organizations and makes treatments more accessible to those suffering from chronic ailments..


Santhigram Foundation
Santhigram Wellness Online – is a Delaware C Corp providing a HIPAA-compliant smart contracts platform for patient records and management with a Software-as-a-Service (SaaS) wellness app for patient diagnostics, health, and monitoring which also provides for data collection and data discovery with tokenized incentives to the user community. It is the digital development arm of the research performed by the Santhigram Foundation.
Santhigram Wellness Online

THE PROBLEM AND THE SOLUTION
The Conventional Medical System
The conventional medical system serves the community in a number of vital functions:
Acute infection control
Surgical correction of acquired and congenital anatomical deformities
Critical care in emergences.
However, the current shortfalls include the following:
Antibiotic resistance
Rise in surgical complications
Adverse drug reactions and side effects
Growing cost of healthcare
Epidemic of lifestyle disorders
Increasing prevalence of psychological disorders
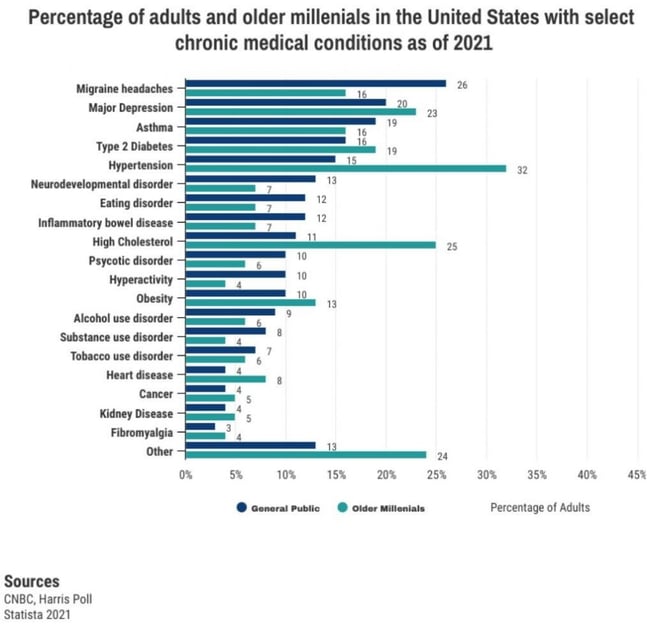
Increasing chronic disorders particularly among older millenials
THE PROBLEM AND THE SOLUTION
Tap image to enlarge
The Conventional Medical System
The conventional medical system serves the community in a number of vital functions:
Acute infection control
Surgical correction of acquired and congenital anatomical deformities
Critical care in emergences.
However, the current shortfalls include the following:
Antibiotic resistance
Rise in surgical complications
Adverse drug reactions and side effects
Growing cost of healthcare
Epidemic of lifestyle disorders
Increasing prevalence of psychological disorders
Increasing chronic disorders particularly among older millenials
Lack of data-driven, scientific studies
Research-based, peer-reviewed scientific studies on the efficacy of Ayurvedic therapies are scattered and sparse.
Existing approaches to therapy are not based upon data-driven, science-based predictive modeling to optimize patient outcomes.
As a result, the general Western population thinks that Ayurveda is either a placebo or folklore without real world evidence.


The Objective
Through the Santhigram Foundation, a non-profit 501(c)(3), research is being conducted to:
Compile pre-existing research published in medical journals and present it to the public via a curated online library;
Perform new research using Whole Person Research (WPR) methods and Pragmatic Trials, conducting data analysis of thousands of Ayurvedic patient questionnaires on health and wellness outcomes, and utilizing sentiment analysis of textual information on patient experiences of Ayurvedic interventions;
Construct statistical models that assess the efficacy of and validate treatments according to condition based upon outcome-based evidence and then build predictive models using machine learning to aid practitioners in the recommendation of precision care.
Validate the cost-benefit analysis of preventive healthcare;
Advocate for Ayurvedic healthcare and allied sciences.
Based upon a controlled, consolidated research study involving tens of thousands of patients, Santhigram Foundation will produce a scientifically-based predictive model for patient wellness, treatment, and care. The results of these studies will facilitate Ayurvedic research, diagnosis, and treatment based on symptoms and causative factors for practitioners, hospitals, researchers, and academia alike.
THE SANTHIGRAM FOUNDATION IS CHANGING THE WAY THAT THE WORLD PERCEIVES AYURVEDA , LENDING A MODERN – DAY SCIENTIFIC VALIDITY TO WISDOM THAT HAS BEEN KNOWN FOR OVER 3,000 YEARS AS AYURVEDA BE COMES MORE MAIN STREAM .
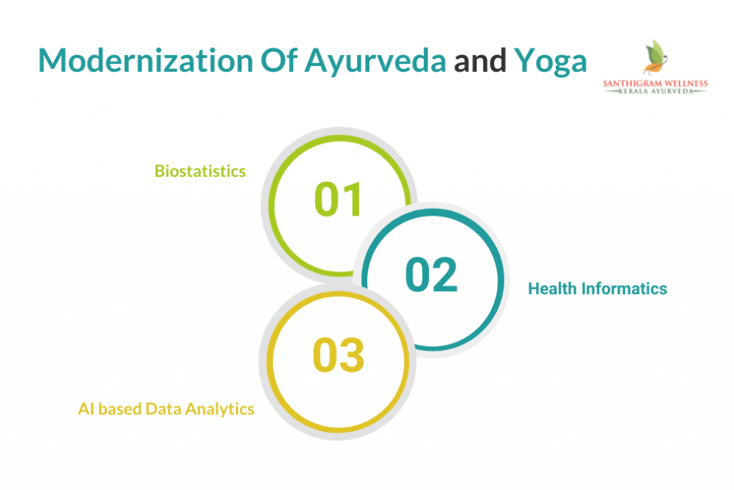
A Breakthrough Approach – The Digital Transformation of Ayurveda
Employing a multidisciplinary team of scientists, statisticians, Ayurveda researchers, and computer scientists using Big Data and machine learning approaches, the Santhigram Foundation is undertaking a body of research that analyzes cause-and-effect relationships that underlie Ayurvedic treatment methods. Santhigram Foundation will statistically analyze patient profile, health, symptoms, conditions, treatment plans, compliance, and outcomes. This data collection provides the basis of a systematic, data-driven research study that correlates actions with outcomes and quantitatively reports the effectiveness of Ayurvedic methods and treatments. Santhigram’s research will be able to provide guidance for practitioners that are based upon peer-reviewed, scientifically validated results. Practitioners can utilize these results to aid in the development of treatment as well as lifestyle plans for optimal patient outcomes. This research will be initially focused upon chronic conditions such as pain, mood disorders, and sleep disorders.
Commercial Application
Through Santhigram Wellness Online, a Delaware C Corp, the research performed in the Santhigram Foundation will be licensed and used towards a commercial application, a Software-as-a-Service (SaaS) platform for patient wellness, including the following:
Wellness diagnostics from a trained practitioner and recommendations that are informed by both doctors and predictive models;
Patient healthcare diagnostics, monitoring and tracking;
Anonymized data collection (which is then used for further research and refinement of predictive models);
Wellness incentives provided to the users through tokenization;
Patient records also kept and managed through a HIPAA-compliant platform accessible by practitioners and patients utilizing smart contracts on the blockchain.
Benefits of The Digital Transformation of Ayurveda
Bringing the methods of precision healthcare to Ayurveda
Generating more patient data and research
More robust scientific analyses and modeling
Better healthcare using better insights
Better monitoring of patient care and outcomes
Reliable, interoperable patient records
Unifying practitioners on a common platform
Building and unifying Ayurveda and Yoga communities
Lowering healthcare costs through prevention
Enhancing the credibility of integrative medicine through data-driven, scientific approaches
METHODOLOGY
Background
In India, 60% of registered physicians are involved in traditional and alternate systems of medicine. There are about 700,000 registered practitioners of traditional medicine, and India has given official recognition to traditional systems of medicine. Medical delivery in most traditional medicine formats is either oral or paper-based, without records in current health databases. Also, lack of information on drug-herbal interactions, limits on what practitioners can cure and absence of digital records act as inhibitors in establishing the efficacy of traditional medicine, although it has been practiced for centuries with documented high outcomes. There are not enough well-controlled clinical trials and systematic research reviews of traditional medicine in comparison with modern medicine to prove that the approaches are beneficial.
Data Collection
Understanding healthcare in an objective, data-centric way involves reliable and reproducible generation of analysis of a large curated dataset. In this study, 10,000+ patients’ data are captured digitally through questionnaire format. The entire dataset is analyzed based on age, sex, region, chronicity, Vikriti, disease morbidity, and comorbidity and reported effectiveness of the treatment. These features are further segregated into different categories to generate a framework of data which are used for analysis.
Meta-Analysis in Ayurveda
Whole Person Research (WPR)
From the National Institutes of Health, research on whole person health in the complementary and integrative spheres emphasizes research on multicomponent interventions that aim to improve health in multiple interconnected domains: biological (including multiple organs and systems), behavioral, social, and environmental.
As a relatively new concept, research on whole person health is different from reduction-based research, which mostly focuses on a single intervention’s impact on one or at most a few physiological systems as separate processes. Understanding how multiple physiological systems interconnect and interact is one of the key challenges for the success of research on whole person health. Complementary and integrative health approaches often are multicomponent interventions or engage multiple therapeutic systems. Their complexity and heterogeneity can require innovative study designs to fully investigate their fundamental science and therapeutic effects.
The National Institutes of Health (NIH), National Center for Complementary and Integrative Health (NCCIH) has embraced the concept of whole person health to underlie its research effort and drive discovery as “supporting the health and well-being of each person across multiple domains—biological, behavioral, social, and environmental—through research on multicomponent nutritional, psychological, and physical approaches to care.” The NCCIH has included the concept of whole person health in its new 5-year strategic plan, with areas of exploration including Ayurveda, Traditional Chinese Medicine, and naturopathy. Areas such as nutritional research and stress management research offer unique opportunities for studying whole person health.
Pragmatic Trials
Schwartz and Lellouch were the first to use the word “pragmatic” in relation to clinical trials in 1967. They defined a pragmatic trial as a trial designed to help chose between care options, as opposed to an explanatory trial which is used to test causal research hypotheses, for example about biological processes.
About 30 years later Roland and Torgerson made the distinction between these two types of trials in a slightly different way, explaining that explanatory trials evaluate efficacy, the effect of treatment in ideal conditions, and pragmatic trials evaluate effectiveness, the effect of treatment in routine clinical practice.
Pragmatic clinical trials are based on data from unselected patients recruited from common clinical practice. These trials therefore bridge the gap between evidence-based medicine and clinical practice. Pragmatic trials seek to investigate whether a treatment works in the clinical setting, preferably on all types of relevant patients.
An ideal pragmatic trial includes an unselected group of patients who are candidates for a type of clinical treatment, with end points and follow-up that to the greatest possible extent take place within common clinical practice. The results provide us with real-world data that can inform the decision on whether or not to introduce a new treatment on a general basis. Pragmatic trials are of interest to decision-makers because these trials also aim to answer questions on the cost-effectiveness of new treatments that are to be introduced in the healthcare service.
Prospective Risk Prediction
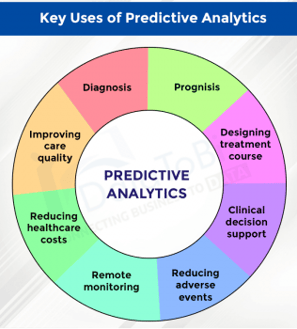
Prospective Risk Prediction is fundamental for the success of proactive disease interventions. The identification of future high-risk scenarios with clinically based rules provides an accurate method for setting intervention levels and maximizes the effectiveness of the intervention.
The complete modelling process, which combines data engineering technology with advanced statistical modelling, can be categorized into four distinct processes:
Data mining and data analysis
Statistical modeling
Assessment of predictive models
What-if calculation
Researchers endeavoring to aggregate and synthesize scientific literature on a particular topic are increasingly conducting meta-analyses. A meta-analysis can be defined as a systematic literature review supported by statistical methods where the goal is to aggregate and contrast the findings from several related studies. Thus, meta-analysis aims to assess the relative effectiveness of several interventions and synthesize evidence across a network of randomized and/or non- randomized clinical trials or other relevant sources of information.
Researchers are also increasingly using real world evidence (RWE) for synthesizing information from nonclinical sources with information from regular randomized clinical trials (RCT). Real world evidence (RWE) can include non-randomized studies, electronic health records, disease registries, and claims data, but are not limited to these. Although RCTs are considered the most reliable source of information on relative treatment effects, their strictly experimental setting and inclusion criteria may limit their ability to predict results in real-world clinical practice. RWE is increasingly used due to its greater potential for generalizability to clinical practice than RCT findings.
The Food and Drug Administration (FDA) recognizes Real-World Data (RWD) as data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources. The reliability of RWD, RWD sources, and resultant analyses are assessed by evaluating several factors as to how the data was collected and that data quality and integrity are sufficient (data assurance).
Meta-Analysis in Ayurveda
Artificial Intelligence (AI) in Risk Prediction
Building the Santhigram’s analytics and AI program includes the following steps:
Acquire data
Social determinants data
Patient-reported data
Unstructured clinical data
Data from Real World Evidence and Pragmatic Trials
Healthcare and clinical partner data
Mobile or IoT device data
Train or refine models by evaluating the models under realistic conditions
Incorporate models into workflow by embedding the insights directly into applications at key decision points
Monitor performance and revisit as more data is consumed and as the environment changes.
AYURVEDA AS A PLATFORM FOR PRECISION HEALTH
The Precision Medicine Initiative (PMI) of the US Government is an attempt to revolutionize healthcare delivery by tailoring preventive and management strategies to an individual’s unique characteristics. This sets the stage for Ayurvedic principles of personalized medicine to be globally adopted for better health.
The strongest and possibly greatest contribution from Ayurveda may be its preventive and promotive healthcare strategies. Our genes, behaviors (such as exercise and eating habits), and environment are all factors that affect our health. The goal of both Ayurveda as well as precision health is to protect our health by measuring these factors and acting on them. Interventions can be tailored to the patient, rather than using the same approach for everyone.
The Santhigram Foundation promotes the application of artificial intelligence and machine learning to Ayurveda research, as it has the potential to improve patient outcomes while also driving operational efficiency. By supporting healthcare providers with predictive machine learning models and insights afforded by Santhigram’s Ayurvedic research, practitioners will have the ability to better forecast adverse health events and adverse episodes and intervene early with personalized care and access to curated information to support a superior patient experience. Prevention and treatment regimens can be more closely tailored to the patient’s genomics, constitution, and condition. Modern-day practices of precision health can merge together with Ayurveda, ushering in a New Age of data-driven, scientifically validated Ayurvedic methods and optimal patient health.

REFERENCES
Patwardhan, Bhushan, et al. Systems Ayurveda: Conceptual Foundation and Logic
Matria Informatics. Predicting High Cost Members in a Disease Management Setting
Langevin, Helene, National Institutes of Health (NIH). Pragmatic Trials Deepens Real-World Understanding of Health Interventions
Kadiroo Jayaraman. Statistical Analysis in Ayurveda Research
Bigelow, Jamieson, et al. Point-of-Care Technologies for the Advancement of Precision Medicine in Heart, Lung, Blood, and Sleep Disorders
Harpreet, Sapna, et al. Big Data Analysis of Traditional Knowledge-based Ayurveda Medicine
Tiwari, Kutum, et al. Recapitulation of Ayurveda Constitution Types by Machine Learning of Phenotypic Traits
The White House. The Precision Medicine Initiative (PMI)
New Age Of Wellness
Explore modern Ayurveda through data-driven insights.
Contact Information
Balance
© 2025. All rights reserved.
